When are concurrent queries initiated?
Correct Answer:
C
The clinical documentation integrity practitioner (CDIP) is reviewing tracking data and has noted physician responses are not captured in the medical chart. What can be done to improve this process?
Correct Answer:
C
According to the AHIMA/ACDIS Query Practice Brief, one of the best practices for a compliant query process is to provide ongoing education to physicians on the importance of documentation integrity, the query process, and the impact of documentation on quality measures, reimbursement, and compliance1. Education can help physicians understand the rationale and expectations for responding to queries, as well as the benefits of accurate and complete documentation for patient care and data quality. Education can also address any barriers or challenges that physicians may face in responding to queries, such as time constraints, technology issues, or workflow preferences1. References:
✑ AHIMA/ACDIS Query Practice Brief – Updated 12/2022
✑ Guidelines for Achieving a Compliant Query Practice (2019 Update) - AHIMA
The clinical documentation integrity (CDI) manager is reviewing physician benchmarks and notices a low-severity level being measured against average length of stay.
What should the CDI manager keep in mind when discussing this observation with physicians?
Correct Answer:
A
According to the AHIMA CDIP Exam Preparation Guide, one of the CDI metrics and statistics that CDI managers should track and interpret is the severity level measured against average length of stay (ALOS)1. This indicator reflects the complexity and acuity of the patient population and the quality of care provided by the hospital2. A low-severity level with a high ALOS may indicate under-documentation or under-coding of the patient??s condition, which may affect the hospital??s reimbursement, risk adjustment, and quality scores3. Therefore, the CDI manager should keep in mind that this indicator is a key factor of measurement for quality reports when discussing this observation with physicians, and educate them on the importance of documenting and coding accurately and completely to reflect the patient??s true severity of illness. The other options are not correct because they do not address the issue of severity level measured against ALOS, or they are not relevant to the CDI manager??s role or responsibility. References:
✑ CDIP Exam Preparation Guide - AHIMA
✑ Demystifying and communicating case-mix index - ACDIS
✑ Severity of Illness: What Is It? Why Is It Important? | HCPro
Which physician would best benefit from additional education for unanswered queries?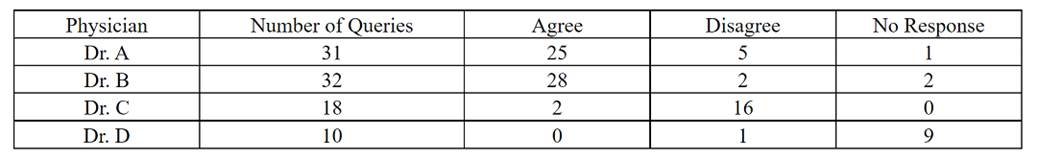
Correct Answer:
D
According to the Documentation Integrity Practitioner (CDIP®) study guide, the physician with the highest number of unanswered queries would benefit from additional education. In this case, Dr. D has the highest number of unanswered queries with 9. Unanswered queries may indicate a lack of understanding, engagement, or compliance with the query process, which may affect the quality and accuracy of clinical documentation and coding1. Therefore, Dr. D would best benefit from additional education for unanswered queries, such as the importance of timely and appropriate query responses, the impact of queries on severity of illness, risk of mortality, and reimbursement, and the best practices for a compliant query practice2. References:
✑ Q&A: What to do with unanswered queries | ACDIS
✑ Guidelines for Achieving a Compliant Query Practice (2019 Update) - AHIMA
An 80-year-old male is admitted as an inpatient to the ICU with shortness of breath, productive yellow sputum, and a temperature of 101.2. CXR reveals bilateral pleural effusion and LLL pneumonia. Labs reveal a BUN of 42 and a creatinine level of 1.500.
The patient is given Zithromax 500 mg. IV, NS IV, and Lasix 40 mg tabs 2x/day. The attending physician documents bilateral pleural effusion, LLL pneumonia, and kidney failure. Two days later, the renal consult documents AKI with acute tubular necrosis (ATN). The correct principal and secondary diagnoses are
Correct Answer:
C
According to the ICD-10-CM Official Guidelines for Coding and Reporting FY 2023, the principal diagnosis is defined as "the condition established after study to be chiefly responsible for occasioning the admission of the patient to the hospital for care"2. In this case, the patient was admitted with shortness of breath, productive yellow sputum, and a temperature of 101.2, which are signs and symptoms of pneumonia. The CXR confirmed the diagnosis of LLL pneumonia, which is a serious condition that requires inpatient care. Therefore, LLL pneumonia is the principal diagnosis.
The secondary diagnoses are defined as "all conditions that coexist at the time of admission, that develop subsequently, or that affect the treatment received and/or the length of stay"2. In this case, the patient had bilateral pleural effusion and kidney failure at the time of admission, which are coexisting conditions that affect the treatment received and/or the length of stay. The renal consult documented AKI with ATN, which is a more specific diagnosis than kidney failure and reflects the severity and etiology of the condition. Therefore, AKI with ATN and bilateral pleural effusion are secondary diagnoses. References:
✑ CDI Week 2020 Q&A: CDI and key performance indicators1
✑ ICD-10-CM Official Guidelines for Coding and Reporting FY 20232